Most of us have either heard of or actually experienced the commonly reported symptoms of the coronavirus disease 2019 (COVID-19) - loss of the sense of taste and smell, fever, cough, sore throat, muscle or bone aches, chills, and headache. However as the pandemic has evolved, GI symptoms characteristic of Functional gastrointestinal disorders (FGIDs) have also started emerging as important clinical manifestations. In fact, in some cases, GI symptoms might be the first signs of COVID-19, even before fever and respiratory symptoms are reported (1).
FGIDs, now called disorders of gut–brain interaction (DGBI), have major economic effects on healthcare systems and adversely affect quality of life. These are common disorders characterized by persistent and recurring GI symptoms that occur as a result of abnormal functioning of the GI tract. The most common and best researched FGID, Irritable Bowel Syndrome (IBS), is characterized by excruciating abdominal pain associated with altered bowel habits of diarrhea, constipation or alternating between both, often triggered by certain types of food. It has been reported that IBS is the second leading cause, after the common cold, for missing work or school (10).
How can COVID-19 infection lead to FGIDs?
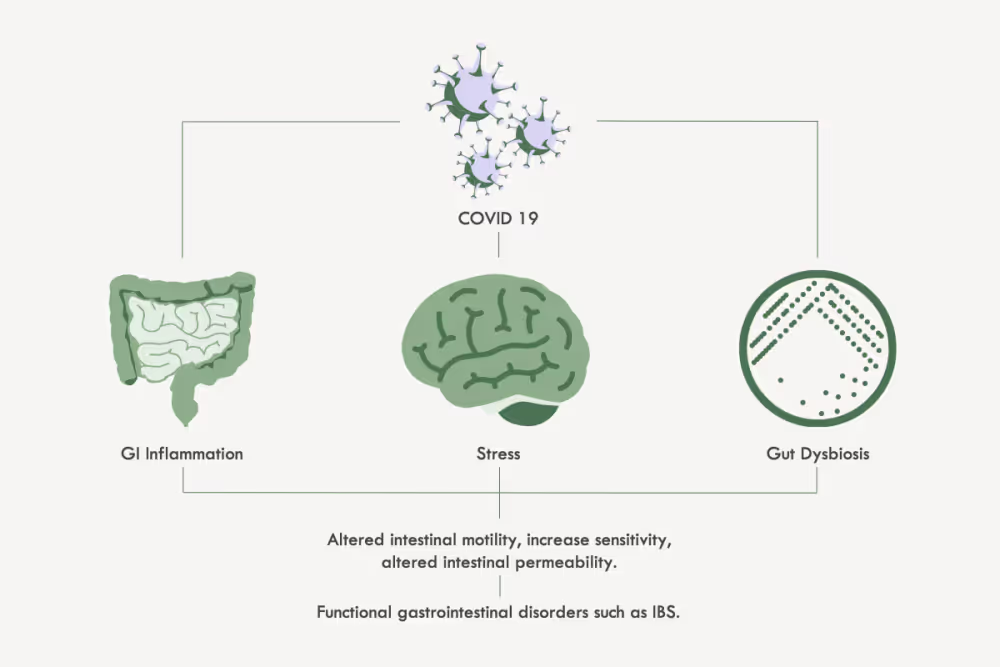
The answer is not entirely clear. However, some evidence points to a role for angiotensin- converting enzyme 2 (ACE2) – a key COVID-19 receptor on the surface of many of our cells and to a COVID-19– induced inflammation in the GI tract. The airways are one of the main sites of COVID-19 entry, where it binds to ACE2 receptors and proliferates while suppressing our immune response. However, ACE2 receptors are also abundantly expressed in the GI tract making it a potential route of COVID-19 infection. COVID-19 invasion of the GI tract has been shown to evoke a strong intestinal inflammatory process which could eventually contribute to the development of persistent GI symptoms (2).
Another contributor could be gut dysbiosis – an alteration in our resident gut microbial communities as a fallout of the various inflammatory molecules produced by our immune cells to tackle the COVID-19 infection in the respiratory tract, or in the gut, or both. In healthy individuals, gut microbes protect the GI tract by (a) deterring pathogenic microbes from colonizing, (b) neutralizing pathogens and, (c) keeping the local immune system in a perpetual vigilant state (3). They also play an important role in the synthesis of vitamins and fermentation of carbohydrates and other undigested nutrients and aid in the delivery of essential nutrients to maintain healthy cells in our colon. A COVID-19 induced imbalance in the number and composition of this resident microbial community can disturb all these processes that support the normal functioning and health of our GI tract.
Interestingly, this microbial perturbation can continue to exist after COVID-19 symptoms resolve leading to persistent gut dysfunction and symptom generation (4). The persistent dysbiosis may contribute to maintaining a chronic state of low-grade intestinal inflammation. This has been associated with increased intestinal permeability, altered gut motility, and increased sensory perception leading to FGIDs/DGBI (8).
COVID-19 and IBS
Some of these gut microbiome changes have been associated with IBS. Specifically, the abundance of anti-inflammatory microbes such as Faecalibacterium prausnitzii others belonging to the Bacteroides group reduces as the severity of COVID infections increases (4). Depletion of such anti-inflammatory microbes has been related to the onset of IBS (5,6).
A subset of patients with acute gastroenteritis caused by viruses have also been shown to develop post-infection IBS (PI-IBS) (7). Researchers thus believe that the development of PI-IBS may follow COVID-19 infection (9).
Another hypothesis proposes that the trigger could be COVID stress. Individual susceptibility to the postinfection and postinflammatory FGIDs/DGBI could be influenced by the presence of pre-existing psychologic disturbances such as anxiety or depression. The COVID-19 outbreak has caused immense stress and anxiety among the general public. Strict measures to counter the pandemic, including physical distancing, have also taken a toll on physical and mental health. Just as GI irregularities can lead to psychological stress, increased anxiety and stress can precipitate FGIDs. Given the high prevalence of psychological impairment during COVID-19, it seems reasonable to speculate an increase in the prevalence and severity of FGIDs, such as IBS, post COVID-19 infection. In fact, 12% of respondents in a recent study reported significant worsening of IBS symptoms during the COVID pandemic (11).
An initial hypothesis first linking COVID-19 infection to the development of IBS and other FGIDs published at the onset of the pandemic in the American journal of Gastroenterology has now been corroborated with clinical data. Conducted by researchers in India and Bangladesh, the study published in November 2021 in the Journal of Gastroenterology and Hepatology, compared the frequency and spectrum of post‐infection‐FGIDs among 208 COVID‐19 patients against 264 historically healthy individuals at 1, 3 and 6-months post COVID infection. The data shows about 9% of patients with COVID‐19 may develop FGIDs ( approximately 5% develop IBS) during the 6‐month follow‐up.
In conclusion, a COVID-19 infection might trigger post-COVID IBS in some patients. The combination of biological aberrations described above coupled with pandemic stress could spawn a surge in FGIDs such as IBS. As daunting as this sounds, knowing how often, when, and why COVID-19 causes GI symptoms could play a significant role in mitigating the social, economic and healthcare burden of the resulting FGIDs. Researchers are already trying to learn more about the long-term effects of COVID-19 on the GI tract (12). As scientists understand the disease better, and COVID-19’s impact on the gut becomes clearer, we will be able to characterize the risk factors for the development of functional post-COVID GI abnormalities. As clinicians become more aware of the possibility of development of FGIDs/DGBI in some patients who have suffered from COVID-19, especially those who had early GI symptoms, such high-risk patients can be given greater attention, screened early, and provided early help in a personalized manner.
References
[1] Schmulson M, Dávalos MF, Berumen J. Beware: Gastrointestinal symptoms can be a manifestation of COVID-19. Rev Gastroenterol Mex (Engl Ed). 2020 Jul-Sep;85(3):282-287.
[2] Effenberger M, Grabherr F, Mayr L, Schwaerzler J, et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut. 2020 Aug;69(8):1543-1544.
[3] Hussain I, Cher GLY, Abid MA and Abid MB (2021) Role of Gut Microbiome in COVID-19: An Insight Into Pathogenesis and Therapeutic Potential. Immunol.12:765965.
[4] Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, et al. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology. 2020 Sep;159(3):944-955.e8.
[5] Barbara G, Grover M, Bercik P, et al. Rome Foundation Working Team report on post-infection irritable bowel syndrome. Gastroenterology 2019;156:46–58.e7.
[6] Barbara G, Cremon C, Stanghellini V. Inflammatory bowel disease and irritable bowel syndrome: Similarities and differences. Curr Opin Gastroenterol 2014; 30:352–8.
[7] Klem F, Wadhwa A, ProkopL J, etal. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: A systematic review and meta-analysis. Gastroenterology 2017;152:1042–54.e1.
[8] Barbara G, Feinle-Bisset C, Ghoshal UC, Quigley EM, et al. The Intestinal Microenvironment and Functional Gastrointestinal Disorders. Gastroenterology. 2016 Feb 18:S0016-5085(16)00219-5.
[9] Schmulson M, Ghoshal UC, Barbara G. Managing the Inevitable Surge of Post-COVID-19 Functional Gastrointestinal Disorders. Am J Gastroenterol. 2021 Jan 1;116(1):4-7.
[10] https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/What-Is-Functional-GI.pdf
[11] Oshima T, Siah KTH, Yoshimoto T, Miura K, Tomita T, Fukui H, Miwa H. Impacts of the COVID-19 pandemic on functional dyspepsia and irritable bowel syndrome: A population-based survey. J Gastroenterol Hepatol. 2021 Jul;36(7):1820-1827.
[12] Hunt RH, East JE, Lanas A, Malfertheiner P, Satsangi J, Scarpignato C, Webb GJ. COVID-19 and Gastrointestinal Disease: Implications for the Gastroenterologist. Dig Dis. 2021;39(2):119-139.


 FODZYME Research
FODZYME Research