If you've ever Googled "how to reset digestive system," irritable bowel syndrome (IBS) may have made it difficult to figure out which "reset" method to try. You've likely come across 3-day cleanses or detoxes that promise a quick fix. But when it comes to IBS, those short resets don't address the root of digestive symptoms, and may even make your symptoms worse.
This article isn't about cleanses or excessive restriction. Instead, we'll focus on holistic, sustainable approaches to gut health by implementing gut-friendly habits that support digestion, relieve symptoms, reduce IBS flare-ups, and help you feel your best in the long term.
What Does a Digestive Reset Mean for IBS?
While short cleanses or detoxes may sound appealing, they don't actually improve gut function (and for people with IBS, have the potential to trigger more symptoms due to excessive restriction or lack of nutritional balance).
A digestive reset for IBS is about creating sustainable habits to help calm your symptoms and promote long-term gut health rather than a short-lived reset. This could look like balancing fiber intake, staying hydrated to keep digestion moving smoothly, eating regular meals, managing stress, or prioritizing high-quality sleep. These small, consistent habits can help promote better gut health over time, without the need for drastic cleanses or detoxes.

Why You May Benefit from a Gut Reset if You Have IBS
People living with IBS often find themselves stuck in an endless cycle of trial and error when it comes to finding a diet that enables them to reduce flare-ups. A gut reset could be beneficial if you're experiencing:
- Feeling overly restricted: If your list of "allowed" foods keeps shrinking, a reset can help you reintroduce variety to your IBS diet while keeping your symptoms under control.
- Confusion about what to eat: A reset may offer clarity and structure so you're not second-guessing every bite of food.
- Persistent gut symptoms: If bloating, pain, or irregularity aren't improving, a reset may help you identify hidden triggers.
- Low energy: Supporting digestion with balanced meals can ensure you're getting the energy and nutrients your body needs to feel its best.
- Bloating or pain during exercise: If you're experiencing workout bloating or abdominal pain after exercising, a gut reset may help you determine which forms of exercise work best for your body.
- Taking a long list of nutritional supplements: If you're taking multiple supplements to help manage IBS symptoms and feel like they're not working, a gut reset could help you get back on track.
Remember, a gut reset isn't about eliminating a long list of foods; rather, it's about getting back to the basics to help promote long-term gut health. While you may need to temporarily eliminate some food triggers, the ultimate goal is to have a varied diet that includes a wide range of foods to ensure you're getting enough calories and essential nutrients.

Signs Your Digestive System Needs a Reset
Our bodies are good at giving us signals when something is out of balance. Some of the most common symptoms of IBS include:
- Persistent bloating that leaves you feeling uncomfortable or overly full.
- Stomach pain or cramping that interferes with daily activities.
- Excess gas that leads to abdominal pain and bloating after eating.
- Irregular bowel movements, such as constipation, diarrhea, or alternating between the two.
- Trouble sleeping because you're gassy and bloated at night.
If you have symptoms of IBS that keep showing up despite your best efforts to get them under control, it may be time to consider a digestive reset focused on restoring balance and supporting gut health.
How to Reset Your Digestive System with IBS
Remember, when it comes to managing IBS symptoms, different strategies will work for different people. This list of strategies is designed as a starting point for managing your symptoms effectively. For a comprehensive management plan, we recommend working with a dietitian for IBS.
Simplify Your Diet with Gut-Supportive Foods
While there's no one "best IBS diet," eating a healthy diet with IBS doesn't have to be complicated. Focusing on simple, whole foods can help keep meals enjoyable while ensuring you get enough dietary fiber, healthy fats, and overall calories.
Here are some of our favorite gut-supportive foods. We've chosen lower-FODMAP options to reduce the risk of triggering symptoms, but if FODMAPs don't trigger your IBS symptoms, feel free to include higher-FODMAP options as well.
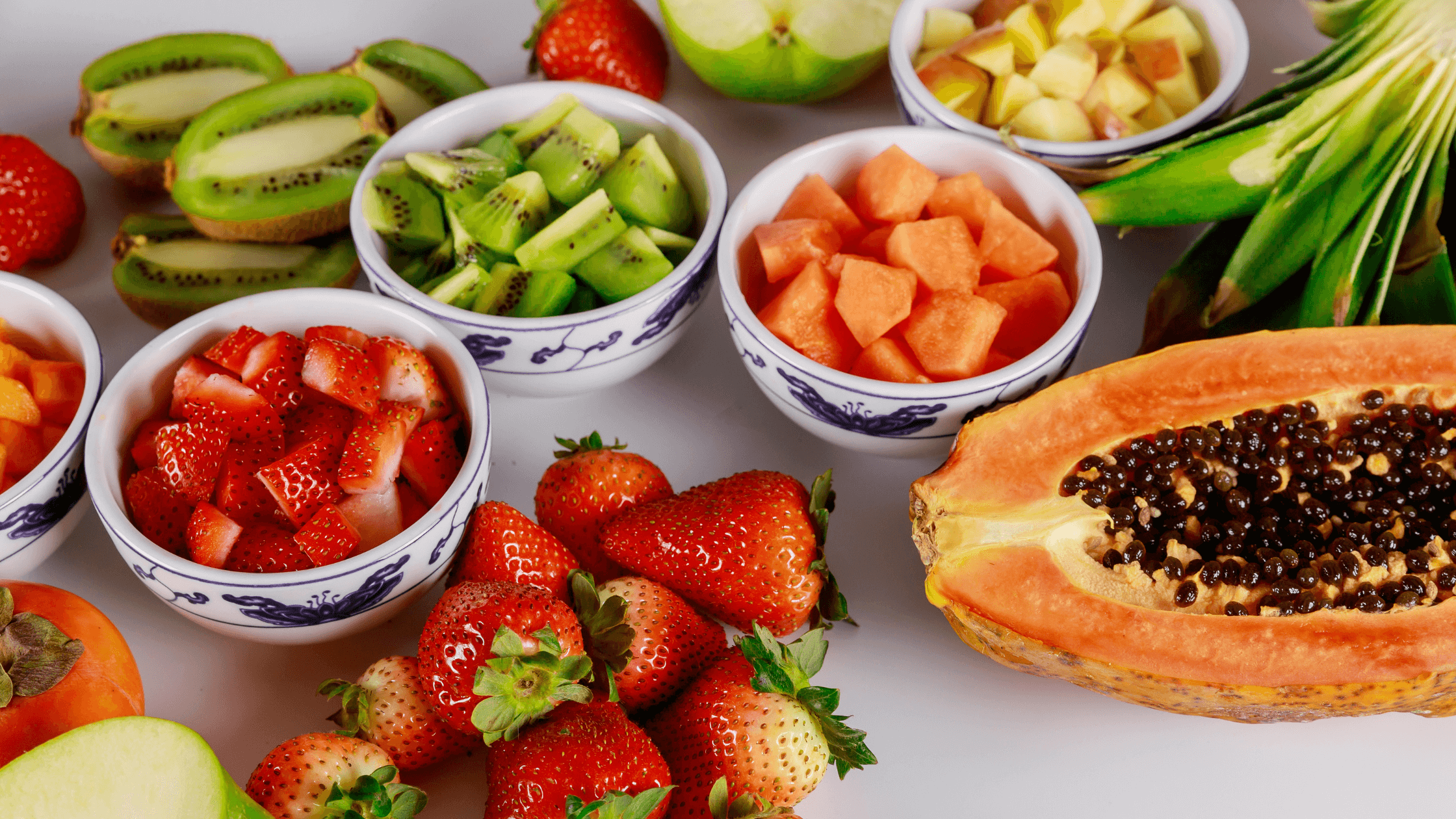
Fruits and vegetables:
- Strawberries
- Blueberries
- Raspberries
- Oranges
- Pineapple
- Kiwi (bonus: Eating two kiwis per day has been shown to improve constipation)
- Zucchini
- Carrots
- Green bell peppers
- Cucumber
- Green beans
Easily digestible proteins:
- Eggs
- Poultry
- Fish and seafood
- Lean cuts of beef or pork
- Firm tofu
- Tempeh
- Canned, drained lentils or chickpeas (most people can tolerate up to ¼ cup per meal, even if they're sensitive to FODMAPs)
- Dairy products like lactose-free milk or lactose-free yogurt
Whole grains and starchy vegetables (carbohydrates)
- Oats
- Brown rice
- Quinoa
- Millet
- Polenta
- Corn tortillas
- Spelt sourdough bread
- Gluten-free bread
- Air-popped popcorn
- Potatoes
- Sweet potatoes (in small amounts)
Healthy fats:
- Olive oil
- Avocado oil
- Macadamia nuts
- Pecans
- Walnuts
- Chia seeds
- Ground flax (up to 1 tablespoon)
- Hemp seeds
- Pumpkin seeds
- Peanut butter
Building meals around these basics can help provide steady energy while being gentle on the digestive system. Try to aim to fill half your plate with vegetables (choose cooked vegetables if you struggle to digest raw vegetables), one quarter with protein, and one quarter with whole grains or starchy vegetables. Then add a source of healthy fats to balance out the meal.
While many different foods can trigger IBS symptoms, certain foods, like fried foods, high fructose corn syrup (HFCS), processed foods, spicy foods, cruciferous vegetables (like Brussels sprouts and broccoli), artificial sweeteners (especially sugar alcohols or polyols), dairy foods containing lactose, and alcohol intake, are more likely to cause IBS attacks (or "flare-ups"). You may need to temporarily limit these foods to get your symptoms under control.
Short-Term Reset: 3-Day Gut Reset Protocol
If you're in the middle of an IBS flare-up, a short "flare care" protocol may be helpful. Here are some at-home remedies to consider trying for a few days to help with symptom management:
- Apply heat to your abdomen: If you're struggling with abdominal pain, try applying a hot water bottle or heat pack to your abdomen for 15-20 minutes. This can help relax cramping muscles and soothe pain.
- Take five deep breaths before eating: Many of us rush into meals without taking the time to get our bodies into "rest and digest" mode. Taking five deep breaths before eating can help activate the parasympathetic nervous system, which prepares your body for digestion. Place one hand on your belly and one hand on your chest. Breathe in for a count of four, feeling your abdomen expand underneath your hand. Then breathe out for a count of four. Repeat five times, or as many times as feels comfortable for you.
- Limit high-FODMAP foods or other known triggers: If you're sensitive to high-FODMAP foods or other IBS trigger foods (like caffeine and alcohol), consider limiting them for a few days to give your digestive system a chance to rest. Keep in mind that long-term restriction of foods can be detrimental to your gut health; therefore, this strategy is only intended to be temporary.
- Increase your intake of soluble fiber: Soluble fiber forms a gel in your digestive tract, which can help with both constipation and diarrhea. Gradually increase your intake of foods rich in soluble fiber, such as oats and ground flax. Fiber supplements containing psyllium husk can also be helpful.
- Stay hydrated: If you're experiencing diarrhea, it's essential to drink plenty of fluids to replace the ones you've lost. If you're experiencing constipation, drinking fluids helps move waste through your digestive tract.
- Consider peppermint oil: Enteric-coated peppermint oil has been shown to help with abdominal pain and global IBS symptoms.
- Try digestive enzymes: Digestive enzymes like FODZYME aid digestion by neutralizing FODMAPs like fructans, lactose, and galacto-oligosaccharides (GOS). This can help reduce symptoms such as gas, bloating, and abdominal discomfort while still enjoying prebiotic-rich foods like onions and garlic, which can promote a healthier gut.
Try incorporating two or three of these strategies into your self-care routine for a few days to see if it helps get your digestion back on track and reduces gastrointestinal symptoms.

Extended Gut Reset: Food, Timing & Lifestyle Alignment
A true digestive reset for IBS is a structured process that takes place over several weeks. While not necessarily a ‘reset,’ the most evidence-based approach is the low FODMAP diet. During this type of dietary management for IBS, you'll replace high FODMAP foods with lower FODMAP alternatives for two to six weeks (until your symptoms are under control) and then reintroduce them to learn your triggers and build a personalized diet.
It's essential to note that the elimination phase of the low FODMAP diet, which reduces your intake of prebiotics, shouldn't be followed long-term, as it may lead to gut dysbiosis (an imbalance of microbes in the gut).

Support Digestion with Enzymes and Gentle Fiber
A high fiber diet helps food and waste move through your gastrointestinal tract. Fiber also acts as food for your good gut bacteria. However, many high fiber foods are also high in FODMAPs. Since FODMAPs resist digestion in the small intestine and pass into the colon intact, they can cause digestive problems in people with food sensitivities when they get fermented by the gut bacteria.
Fortunately, digestive enzyme supplements like FODZYME can help break down FODMAPs, reducing IBS symptoms such as gas, bloating, and abdominal pain. This enables you to include high FODMAP foods in your diet without worrying about triggering symptoms.
Here are some high-fiber foods that are gentle on the digestive system:
- Oats (rolled or quick oats, not steel cut)
- Rice
- Quinoa
- Kiwi
- Oranges
- Strawberries
- Bananas (firm)
- Papaya
- Carrots
- Zucchini (peel the skin off and cook it for an even gentler option)
- Potatoes
- Chia seeds
- Ground flax
- Psyllium husk
If you're not used to eating a lot of fiber, add 2 to 3 grams of fiber daily to give your digestive system a chance to adjust. This will reduce the likelihood of experiencing gas and bloating related to fiber intake.

Manage Stress and Mind Your Meal Patterns
Food is only one piece of the IBS puzzle. To truly "reset" your gut and improve IBS symptoms, it's important to adjust certain lifestyle factors such as:
- Eating at regular intervals: Aim for three balanced meals per day, with snacks as needed. Skipping meals or eating very large meals can be triggers for IBS symptoms, so it's important to establish a regular eating pattern to get lasting symptom relief.
- Incorporate gentle movement: Walking, stretching, or yoga can help regulate digestion without stressing your gut.
- Prioritize sleep: Research shows that disturbed sleep can worsen IBS symptoms. Try to prioritize a calming nighttime routine to promote restorative sleep.
- Manage stress: Stress management techniques, such as mindfulness meditation, journaling, or breathing exercises, can help calm the gut-brain connection.
- Try a probiotic: Probiotics help restore beneficial bacteria to your gut. However, not all probiotic supplements work for IBS. It's best to consult with a doctor, pharmacist, or dietitian to help you choose an effective probiotic that has been shown to relieve symptoms of chronic digestive diseases like IBS.
This holistic approach creates a solid foundation for long-term gut health.

Reintroduce Foods Mindfully After the Reset
You'll follow the elimination phase with a structured FODMAP reintroduction to identify which foods and portion sizes you can tolerate. This structured approach helps reduce symptoms in the short term while creating a long-term eating plan that's tailored to your unique food tolerances.
During food reintroduction, you can also start to add back non-FODMAP food triggers, such spicy and fatty foods, in moderation. It can be helpful to keep a food diary during this time so you can see the relationship between your symptoms and different foods.
How Long Should an IBS Digestive Reset Last?
Ideally, the elimination phase of the low FODMAP diet should last no longer than six weeks (and if you haven't noticed an improvement in your symptoms after two weeks, it's generally best to discontinue the low FODMAP diet). Reintroduction can take eight to twelve weeks, depending on how often you develop symptoms during food challenges.
Beyond the low FODMAP diet, other principles of a digestive reset can be followed longer-term, such as focusing on gentle fiber, mindful eating techniques and stress management.
When to Seek Professional Support
While many people can improve their digestion by making diet and lifestyle adjustments, there are times when professional support is needed to help manage IBS attacks. Consider reaching out to a doctor or registered dietitian if:
- Your symptoms are severe, frequent, or worsening despite making diet and lifestyle changes.
- You notice red flag symptoms like unintentional weight loss, blood in your stool, or persistent vomiting.
- You feel overly restricted and aren't sure which foods you should eat (over-restricting your diet can lead to nutritional deficiencies and social isolation).
- IBS symptoms are negatively affecting your mood, energy levels, or quality of life.
- You need guidance on following or personalizing the low FODMAP diet.
- You're pregnant and experiencing IBS symptoms (elimination diets are typically not recommended during pregnancy and other high-risk life stages).

Working with a gastroenterologist or IBS-trained dietitian can help you rule out other digestive diseases (like celiac disease and inflammatory bowel disease) and create a personalized plan to support long-term digestive health.
Reset Your Gut, Regain Control of IBS
Managing IBS doesn't mean avoiding every food you love. With the right strategies — and tools like FODZYME — you can enjoy more food freedom and fewer symptoms.
Try FODZYME today and take the first step towards expanding your diet.