While it can be an extremely effective way to manage the symptoms of irritable bowel syndrome (IBS), navigating the low FODMAP diet for beginners can feel overwhelming. From understanding the different FODMAP groups to learning what your individual triggers are, there's a lot of information to take in. This article will provide you with basic knowledge of the low FODMAP diet so you can implement the principles of this elimination diet with confidence.
Know Your FODMAPs
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. They're a group of short-chain carbohydrates (fermentable sugars) that are poorly absorbed in the small intestine. Instead, they enter the large intestine intact. Here, the gut bacteria ferment them, leading to the production of gas and, in some cases, pulling water into the large intestine. In susceptible individuals (such as people with IBS who have a FODMAP intolerance), this can lead to uncomfortable digestive problems like gas, bloating, stomach pain, stomach cramps, and altered bowel habits.
While we review the different groups of FODMAPs in more detail in our guide to FODMAPs, here's a brief overview of the different FODMAP groups:
- Fructans (a type of oligosaccharide)
- Galacto-oligosaccharides, or GOS (another type of oligosaccharide)
- Lactose (a disaccharide)
- Excess fructose (a monosaccharide)
- Mannitol and sorbitol (polyols, or sugar alcohols)

Different foods contain different FODMAP groups, and some foods contain multiple types of FODMAPs. Here are some common sources of each FODMAP group:
- Fructans: Wheat, onions, garlic, oat milk
- GOS: Black beans, red kidney beans, pinto beans, baked beans, cashews, pistachios, oat milk
- Lactose: Dairy milk, yogurt, ice cream, frozen yogurt, soft cheeses (like cottage cheese), sour cream, evaporated milk
- Excess fructose: Apples, ripe baby bananas, grapes, mango, pears, broad beans, high fructose corn syrup (HFCS), butternut squash (in large portions)
- Mannitol: Celery, mushrooms, watermelon
- Sorbitol: Apples, pears, stone fruits (many fruits high in sorbitol are also high in excess fructose), canned coconut milk (in large portions), many foods with artificial sweeteners (like gum and sugar-free candy)
During the elimination phase of the low FODMAP diet, you'll swap out these high FODMAP foods for lower FODMAP options.

The low FODMAP diet plan has three distinct phases: Elimination, reintroduction, and maintenance.
- Elimination: During this phase, you'll replace high FODMAP foods with lower FODMAP alternatives to create a diet low in FODMAPs. The purpose of this phase is to get your symptoms under control and learn whether you have a FODMAP intolerance. It typically lasts two to six weeks, depending on how much time it takes for you to get symptom relief.
- Reintroduction: During the reintroduction phase, you'll reintroduce foods with FODMAPs back into your diet one FODMAP group at a time to identify foods and portions that trigger your symptoms. This phase lasts eight to twelve weeks (as you need to wait a few days between food challenges) and is an extremely important step in the low FODMAP diet. Remember, FODMAP intolerance doesn't mean you're intolerant to all FODMAP groups. Most people can tolerate some FODMAPs; it's just a matter of finding out which ones.
- Maintenance (Personalization): During this phase, you'll take what you learned during the reintroduction phase to create an eating plan based on your individual tolerance and food triggers. However, it's important to retest your FODMAP triggers every three to six months, as FODMAP tolerance can change over time.
Unfortunately, many people see symptom relief when reducing their intake of high FODMAP foods and end up stuck in the elimination phase for an extended period. However, this is not recommended, as FODMAPs are prebiotics — food for your good gut microbes.

While we're still learning about the effects of following a low FODMAP diet long term, reducing your intake of FODMAPs (i.e., prebiotics) could be detrimental to your overall gut health. For example, a study published in 2021 found that even temporary restriction of FODMAPs led to reductions in the amount of Bifidobacteria (one of our good gut bacteria).
Since the low FODMAP diet is very restrictive, it's not appropriate for everyone, and can significantly impact quality of life. If you have a history of disordered eating or are currently following another restrictive diet, a simplified low FODMAP approach where you only eliminate the highest FODMAP foods could be a better option.
It's best to work with a healthcare professional like a registered dietitian to ensure you're meeting your nutritional needs and do not experience excessive weight loss while following the low FODMAP diet.
Prepare for Low-FODMAP Success with Meal Planning & Support
So, you've decided to try the low FODMAP diet to see if FODMAPs are triggering your IBS symptoms. Here are some tips to help set you up for success.

Stock Up on Low-FODMAP Staples
One of the best ways to ensure you have plenty of low FODMAP staples available is to create a shopping list with low FODMAP foods you enjoy. Here are some low FODMAP staples to consider adding to your list:
- Fruits: Blueberries, raspberries, strawberries, kiwi fruit, mandarin oranges, papaya, passionfruit, pineapple
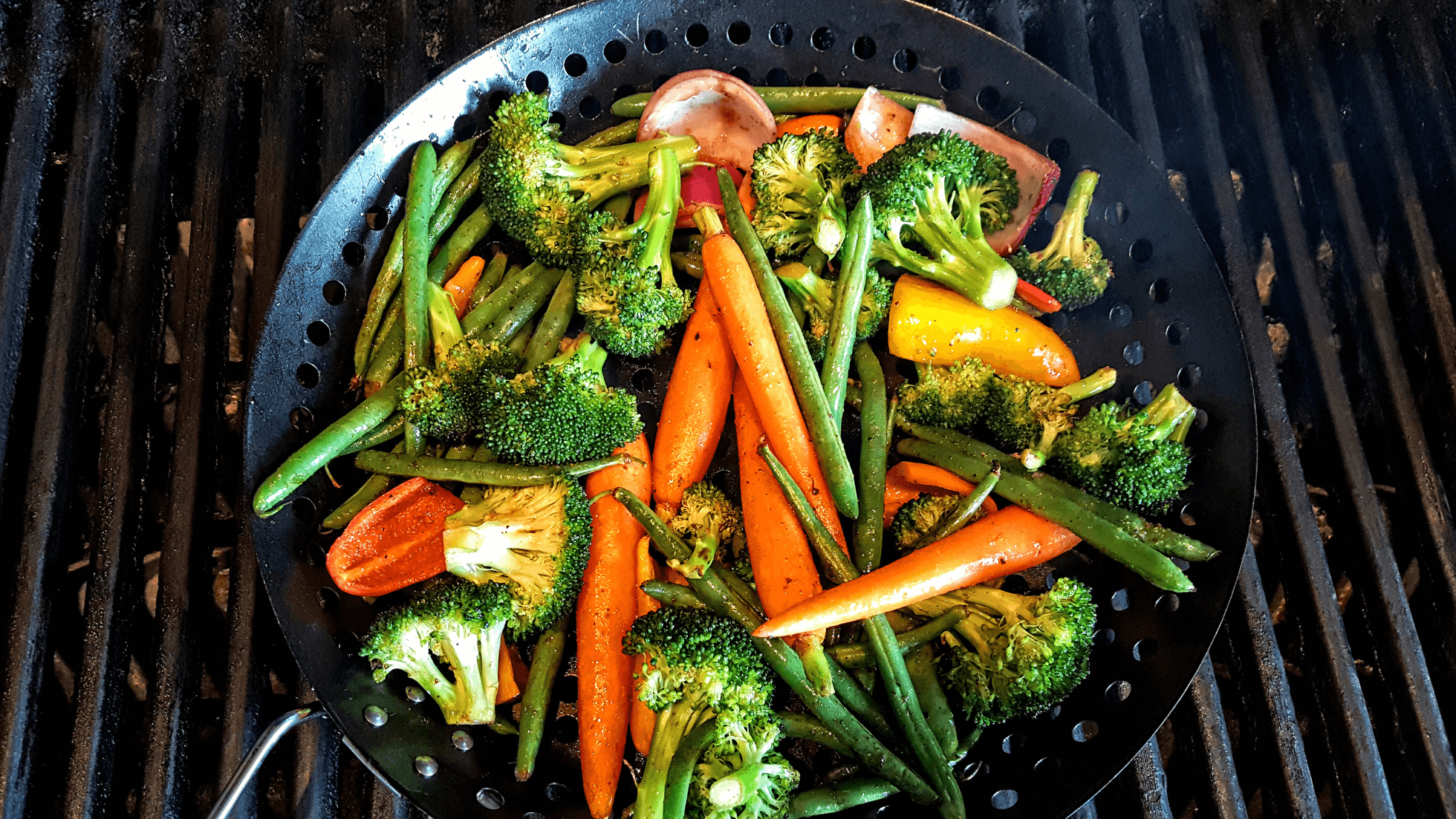
- Vegetables: Green beans, green bell peppers, broccoli (heads only), carrots, collard greens, cucumber, lettuce, spring onions (green tops only), parsnips, snow peas, sugar snap peas, potatoes, radishes, spinach, Swiss chard, zucchini, sweet potatoes (in small servings)
- Grains: 100% spelt sourdough bread, many gluten-free products (like bread, pasta, and tortillas), millet, rice vermicelli noodles, rolled oats, quinoa, rice, corn tortillas, popcorn, rice cakes
- Proteins: Chicken, turkey, fish, shrimp, beef, lamb, pork, eggs, firm tofu, tempeh, canned chickpeas (up to ¼ cup per meal), canned lentils (up to ¼ cup per meal), whey protein isolate, eggs and egg white protein, rice protein
- Dairy and alternatives: Lactose-free milk, lactose-free yogurt, low-lactose cheeses (like cheddar), almond milk, soy milk (if made from soy protein), macadamia milk, hemp milk, rice milk
- Nuts and seeds: Hazelnuts, macadamia nuts, peanuts, pecans, walnuts, chia seeds, hemp seeds, flaxseed, pumpkin seeds, sesame seeds, sunflower seeds
- Fats and oils: Avocado oil, canola oil, coconut oil, olive oil, sunflower oil, sesame oil, margarine, butter
- Condiments, sauces, and spices: Most spices (except garlic and onion powder), most fresh and dried herbs, mayonnaise, horseradish, tahini, tomato pasta, BBQ sauce, fish sauce, soy sauce, sriracha, tamari, mustard, peanut butter, vinegar
- Low FODMAP sweeteners: Allulose, brown sugar, beet sugar, demerara sugar, dextrose, glucose syrup, maple syrup, icing sugar, monk fruit extract, rice malt syrup, stevia, sucralose, white sugar
This list is just an overview, and there are many other low FODMAP foods that you can include in your grocery list. To learn more about which low FODMAP foods you can include during the elimination phase, consider downloading the Monash FODMAP app. This app allows you to search for foods that are lower in FODMAPs. It also tells you which FODMAP groups a food has, which is essential information to have for the reintroduction and maintenance phases of the low FODMAP diet.

Plan Simple & Safe Meals for the Week
Once you've compiled your grocery list and stocked up on low FODMAP essentials, it's time to plan easy low FODMAP recipes so you're prepared for the week ahead.
Here are some dietitian-approved dishes to get you started:
- Breakfast: Scrambled eggs with spelt sourdough toast and strawberries; lactose-free Greek yogurt with homemade low FODMAP granola and blueberries; smoothie made with lactose-free milk, unripe banana, maple syrup, and whey protein isolate.
- Lunch: Grilled chicken breast with quinoa and roasted zucchini; canned tuna with mayo or olive oil on gluten-free bread, cucumber slices, and kiwi fruit; turkey wraps with gluten-free tortillas, Swiss cheese, lettuce, and a side of orange slices.
- Dinner: Baked salmon with brown rice and sauteed green beans; lean beef patty on a lettuce wrap with a side of polenta and roasted carrots; baked cod with mashed potatoes and sauteed kale (<1.5 cups).
- Snacks: Boiled eggs with rice crackers and cucumber slices; sourdough toast with peanut butter and banana slices (firm, unripe); rice cakes with macadamia nut butter and sliced strawberries.
You may find it helpful to create a spreadsheet or list of your meals for the week. Having your planned meals written down will help remind you of your meal plan and may make it easier to stick to low FODMAP foods.

Set Expectations with Your Healthcare Team
Before embarking on a low FODMAP diet, it's crucial to rule out other digestive disorders like small intestinal bacterial overgrowth (SIBO), inflammatory bowel disease (IBD), and celiac disease. Once those digestive disorders have been ruled out, you can start the low FODMAP diet.
While research shows that up to 86% of people with IBS may find relief with a low FODMAP approach, there are still some people for whom FODMAPs aren't a symptom trigger. If you don't notice any changes in your digestive symptoms (like reduced bloating, gas, or abdominal pain) after two weeks of following a low FODMAP diet, it's possible that FODMAPs aren't responsible for your symptoms. If this is the case, it's best to stop the low FODMAP diet to avoid unnecessary restriction so you're not compromising your digestive health.
If it turns out that FODMAPs aren't an IBS trigger for you, other approaches (like gut-directed hypnotherapy and cognitive behavioral therapy) may be better options for you. It's best to explore these treatments under the guidance of a trained health professional.
An Elimination Phase Roadmap for the First Two Weeks
No matter how prepared you are, embarking on the low FODMAP diet can feel daunting. We've created a roadmap for the first two weeks to ensure you understand common low FODMAP challenges (and how to overcome them) and how to build a balanced low FODMAP meal.
Daily Eating Pattern & Portion Tips
When it comes to planning your low FODMAP meals, it can be helpful to use the balanced plate method to ensure you're getting enough protein, dietary fiber, and other nutrients:
- Fill one-half of your plate with low FODMAP vegetables
- Fill one-quarter of your plate with low FODMAP protein
- Fill one-quarter of your plate with low FODMAP grains or starches
It's also important to include a source of healthy fats (like olive oil) in your meals. Lactose-free dairy products and fruit can also be included as part of a balanced meal.
Portion size is also important. Certain foods can be low FODMAP in smaller amounts, but become high FODMAP as the portion size increases. Use the Monash FODMAP app to check the allowed portion sizes for different foods.

And finally, ensure you're eating at regular intervals. Some research shows that an irregular meal pattern is associated with IBS prevalence. If your eating habits involve skipping breakfast and having a small lunch, only to eat a huge meal at dinner, you may end up experiencing worsened symptoms. Instead, aim for three main meals daily, with snacks in between based on your individual hunger levels.
Common Early Hurdles and How to Overcome Them
Despite your best efforts and preparation, you may end up facing some of the following hurdles on the low FODMAP diet:
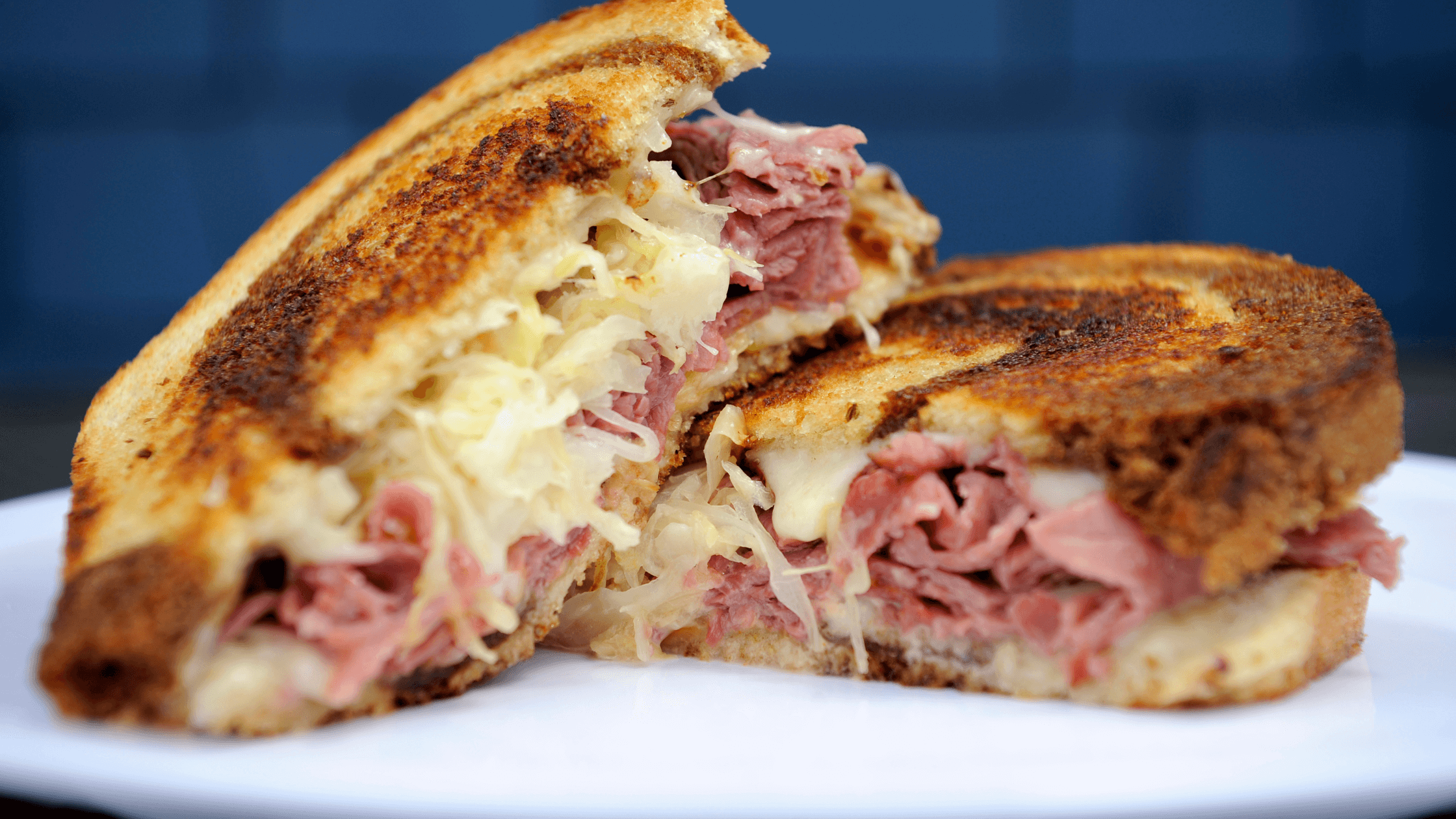
- Accidentally eating FODMAPs in packaged foods: Packaged foods often contain hidden sources of FODMAPs. Some common high FODMAP ingredients to look out for include high fructose corn syrup, honey, agave syrup, sorbitol, mannitol, maltitol, xylitol isomalt, inulin, chicory root extract, fructo-oligosaccharides (FOS), wheat, milk solids, milk powder, fruit juice concentrate (e.g., apple, pear, mango, peach), dried fruits, onion powder, and garlic powder.
- FODMAP stacking: FODMAP stacking is the cumulative build-up of FODMAPs in the digestive tract. Even if you're choosing low and medium-FODMAP foods, eating multiple portions of these foods at the same meal could result in digestive symptoms. To avoid FODMAP stacking, ensure you're eating a varied diet with minimally processed foods from all different food groups.
- Social pressure: Food is a huge part of how we socialize, but it can be challenging to eat out on the low FODMAP diet. Still, it's not impossible. With some preparation (and even practice explaining why you’re on the diet), you can enjoy socializing at restaurants or gatherings where food is on offer.
Remember, accidentally eating FODMAPs doesn't erase the work you've done to reduce your FODMAP intake. Simply return to low FODMAP eating for the remainder of the elimination phase.

Symptom Tracking Basics
If your symptoms are similar before and after the low FODMAP diet, you may need to try keeping a food and symptom log to help pinpoint the origin of your symptoms. While the Monash FODMAP app has a diary function, you can also keep a simple log in your notes app or even use a pen and paper.
Here are some pieces of information to include in your log:
- What you ate/drank, including portion sizes, timing, and preparation method
- Symptoms, including type, severity (on a scale of 0–10), timing (e.g., immediate, 30 minutes after eating, next day), bowel movements (frequency and consistency using Bristol Stool Chart)
- Sleep (hours and quality)
- Stress/mood (on a scale of 0–10)
- Exercise/movement (type, intensity, and duration)
- Menstrual cycle (if applicable; include phase, day, and symptoms)
- Travel/routine changes (e.g., skipped meal, time zone shift)
- Medications and supplements
- Other therapies (massage, acupuncture, etc.)
Patterns often emerge with consistent logging for at least two to four weeks. Many people with IBS find that sleep quality and stress are just as important as what they eat when it comes to managing symptoms.
How to Reintroduce FODMAPs After the Elimination Phase
Reintroducing FODMAPs so you can learn which FODMAP groups trigger your symptoms is one of the most important steps in this elimination diet. Here are some basic tips for FODMAP reintroduction:
- Keep your baseline diet low FODMAP for the entirety of the reintroduction phase
- Reintroduce each FODMAP group separately by using specific test foods that only contain one FODMAP group (the Monash app will guide you on which ones)
- Use two or three increasingly larger portion sizes for each test food to assess your FODMAP threshold accurately
If you experience symptoms during the reintroduction phase, give your gut time to rest before moving on to the next challenge food. Ideally, wait for two or three symptom-free days before moving on with reintroduction.
Eating Out & Social Life as a Low-FODMAP Beginner
While it can feel easier to avoid eating out to ensure you don't accidentally eat high FODMAP foods, you can enjoy an active social life — even if you're following the low FODMAP diet. Here are some tips for managing take-out, date night, and social gatherings on the low FODMAP diet.
Fast-Casual and Take-Out Strategies
Here are some fast food dining tips to keep in mind before your next fast-casual meal:
- Check the menu ahead of time: Look online to find dishes (or call ahead if needed) with simple ingredients and fewer sauces.
- Keep it simple: Choose grilled, baked, or steamed proteins with plain sides.
- Swap sides: Request low FODMAP swaps like plain rice, baked potato, or a side salad with plain vinaigrette.
- Ask about seasonings: Avoid dishes with garlic, onion, marinades, or spice blends. Instead, stick to salt, pepper, lemon/lime, and herbs.
- Look for "build-your-own" options: Sushi, tacos, or salad bars can be customized with suitable ingredients.
- Consider using digestive enzymes: Digestive enzymes that break down FODMAPs can help you enjoy high FODMAP meals without the digestive side effects.
Date Nights & Social Gatherings
Navigating date nights and social gatherings can feel overwhelming, but it doesn't have to. By researching restaurants ahead of time, letting your date know about your dietary restrictions, and bringing your own low FODMAP dishes to potlucks, you can enjoy socializing without having to worry about digestive symptoms.
Using Digestive Enzymes for Added Flexibility
While the low FODMAP diet can be helpful for managing symptoms, sometimes, you just want to eat a meal that has garlic or cream in it. Fortunately, digestive enzymes like FODZYME can help break down the short-chain carbohydrates that can trigger symptoms.
FODZYME contains three enzymes to break down FODMAPs:
- Lactase (for breaking down the lactose in dairy products)
- Alpha-galactosidase (for breaking down the GOS in legumes and certain nuts)
- Fructan hydrolase (for breaking down the fructans in wheat, onions, and garlic)
When you sprinkle FODZYME on your meal, it gets to work breaking down the FODMAPs before they even reach your large intestine, helping to control digestive symptoms like gas, bloating, and abdominal pain.

